Genital itching is easy to brush off. But it’s often an early sign of something more serious in clinical settings. Whether it’s a sharp sting when you urinate or a persistent itch with no visible rash, these symptoms are frequently linked to inflammation caused by a sexually transmitted infection (STI).
Most STIs develop without noticeable symptoms, which is why they spread quickly. According to the World Health Organization, more than 1 million curable STIs are acquired every day by people aged 15 to 49. Each year, chlamydia, gonorrhea, trichomoniasis, and syphilis account for nearly 374 million new cases, many with no clear warning signs. Sometimes, itching is the only early clue, so it should be taken seriously.


This article explains what STDs cause itching and white discharge, how to tell them apart from non-infectious issues, and when to take action.
Let’s dive in!

What STDs commonly cause itching?
When genital itching is the first symptom, the infections highlighted in this section are most likely to be responsible. Each should be taken seriously and ruled out with proper testing. Here are the STDs that cause itching in males and females.
Chlamydia
Chlamydia trachomatis often causes no symptoms, especially in its early stages. However, when symptoms do appear, they tend to result from inflammation of the urethra (urethritis) or cervix (cervicitis), which may lead to:
- A tingling or itchy sensation during urination
- Irritation at the urethral opening (jeuk penis / jeuk aan eikel)
- Discomfort during sex
- Watery or cloudy discharg
In men, chlamydia-related urethritis can mimic fungal infections or allergic reactions, making proper testing critical. Left untreated, it may lead to epididymitis or prostatitis.
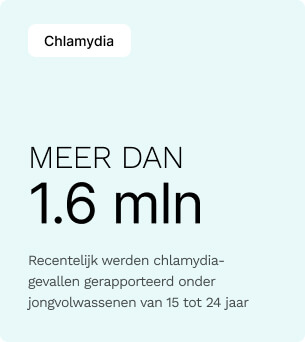
In the United States alone, over 1.6 million chlamydia cases were reported recently, making it the most common notifiable STI among young adults aged 15 to 24.

Genital Herpes (HSV-1 or HSV-2)
Herpes simplex virus causes painful blisters, but itching typically precedes an outbreak and may persist without visible lesions. Early or recurrent symptoms include:
- Localized itching or burning in the penis, vulva, or anus
- Tingling along nerve pathways (sciatic/genital distribution)
- Small red bumps that evolve into fluid-filled blisters
- Skin sensitivity after lesions resolve
Herpes often follows a pattern: itch > blisters > crust > healing. Even without active sores, viral shedding can still occur.
Globally, an estimated 846 million people aged 15–49 are living with genital herpes (HSV‑2), and in the U.S., about 1 in 6 adults carry the virus, most without knowing it.


Trichomoniasis
Caused by the parasite Trichomonas vaginalis, this STD is one of the most common STDs that cause itching in females, often leading to a particularly irritating form of vaginitis or urethritis. In women, symptoms include:
- Vulvar itching (jeuk vagina), especially during urination
- Thin, frothy, yellow-green discharge with a strong odor
- Vaginal burning or soreness
In men:
- Itching inside the urethra or along the shaft (jeuk balzak / jeuk penis)
- Occasional penile discharge
- Post-ejaculatory irritation
Trichomoniasis may increase susceptibility to HIV transmission and requires a specific lab test, as it’s not always detected via standard STD panels.



Trichomoniasis remains widely underdiagnosed despite causing over 156 million new cases each year, with up to 70% of people showing no symptoms.


Gonorrhea
Gonorrhea, caused by Neisseria gonorrhoeae, can lead to intense irritation in the genital tract due to an aggressive immune response. Common symptoms include:
- A sharp burning or itching sensation during urination
- Urethral discharge (often yellow or green)
- Itching or swelling of the foreskin or glans (jeukende eikel / ontstoken voorhuid)
In women, it may manifest as itching around the vaginal opening, increased discharge, or pelvic pain. Because gonorrhea can also infect the rectum or throat, itching in those areas may be a clue.
In the Netherlands, gonorrhoea has surged. Over 13,853 cases were reported at Sexual Health Centres in 2023, including a 78% jump among women and a 51% rise among heterosexual men compared to 2022.


Syphilis
Syphilis progresses in stages, and while the primary sore (chancre) is usually painless, itching may develop during the secondary stage, when the infection spreads systemically.
Typical signs include:
- A non-itchy sore that later progresses to a rash
- Red or brownish spots on the palms, soles, genitals, or trunk
- Generalized itchiness from systemic rash
- Patchy hair loss or mucous membrane lesions
If you notice itchy rashes that don’t resolve and you’ve had unprotected sex, syphilis testing should be part of your diagnostic workup.
Syphilis has resurged in recent years, with over 209,000 U.S. cases of primary and secondary syphilis reported in 2023. In Europe, syphilis cases also rose sharply—about 41,000 cases were confirmed, underscoring a pan‑continental public health concern.


Non-STD causes of genital itching
Not all cases of genital itching are caused by a sexually transmitted disease. In fact, there are many people with symptoms like itching on the glans, itching on the scrotum, or itching in the vagina that are dealing with non-infectious conditions. Here are some of the most common non-STD causes that can mimic or overlap with STD symptoms.
Candida Infection (Yeast Infection)
Cause: Overgrowth of Candida albicans, a naturally occurring yeast.
While often associated with women, candida infections also affect men, especially under the foreskin or in warm, moist environments. Symptoms can include:
- Persistent itching or burning around the penis or vulva
- Red, shiny, or peeling skin (red glans / chafed penis)
- White, clumpy discharge (in women)
- Small red bumps or a blotchy rash (red spots on the glans after sex)
- Pain during sex or urination
In uncircumcised men, yeast can build up under the foreskin (itching under the foreskin) and cause balanitis. A swab test can confirm the diagnosis, and antifungal treatment usually resolves it quickly.




Allergic reactions and irritation
Cause: Skin sensitivity to soaps, detergents, fabrics, latex, or shaving.
Contact dermatitis in the genital area is prevalent and often misread as an STD. Itching may occur immediately after contact or develop gradually with repeated exposure. Common irritants include:
- Scented body wash, fabric softeners, or laundry detergent
- Latex condoms or personal lubricants
- Tight synthetic underwear
- Shaving, especially without proper lubrication or post-care
The resulting symptoms—itchy scrotum, dry skin on the penis, or itching in the pubic area in men—may resemble infection but usually resolve when the trigger is removed. In some cases, a steroid cream or antihistamine may be needed.
Balanitis (Glans Inflammation)
Cause: Poor hygiene, yeast overgrowth, or irritants trapped under the foreskin.
Balanitis refers to inflammation of the glans (glans penis) and is more common in uncircumcised men. It can be triggered by:
- Soap residue or failure to rinse properly
- Candida or bacterial infection
- Accumulation of smegma (natural oils and debris)
- Tight foreskin (phimosis) restricting airflow
Symptoms include:
- Redness or swelling of the glans (cause of red glans)
- Itching, especially under the foreskin (itching under the foreskin)
- Painful urination or pulling back the foreskin
- Foul odor or discharge

Left untreated, balanitis can progress to more serious infections or scarring. Good hygiene, without overwashing, is key to prevention.



Visual symptoms to watch for (besides itching) and related STDs
While itching often brings people to seek help, it rarely appears in isolation. Visual symptoms such as redness, rashes, or unusual skin changes can offer critical clues about what’s happening. Here are some of the most common signs to look out for, what they might indicate, and when testing is essential.


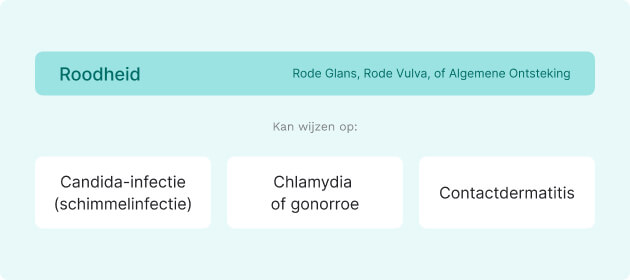
Redness (Red Glans, Red Vulva, or General Inflammation)
Redness can reflect irritation, inflammation, or infection. It may appear as:
- Diffuse redness across the head of the penis (glans) or vaginal opening
- Localized red patches or blotchy discoloration
- Accompanying swelling or heat
Possible causes include:
- Candidiasis (yeast infection): red, shiny skin with discomfort
- Chlamydia or gonorrhea: inflammation of the urethral opening or cervix
- Contact dermatitis: from condoms, soaps, lubricants, or sweat buildup
Persistent redness, primarily if tender or spreading, should be evaluated.
Bumps (raised lesions or lumps on the genitals)
Genital bumps vary in texture, color, and cause. Consider the following:
- Herpes simplex virus (HSV): tingling or itch followed by blisters or ulcers
- Genital warts (HPV): painless, flesh-toned growths, often in clusters
- Molluscum contagiosum: small, dome-shaped bumps with a central dimple
- Syphilis: a single, firm sore (chancre) that’s usually painless
The nature of the bump, whether painful, clustered, or ulcerated, offers essential diagnostic clues.

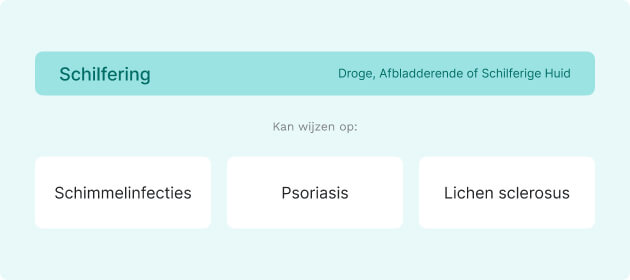
Flaking (dry, peeling, or scaly skin)
Flaking or scaling of genital skin can occur with:
- Fungal infections: often red, itchy, and ring-like in appearance
- Psoriasis: well-defined plaques that may crack or bleed
- Lichen sclerosus: smooth white patches that thin and scar over time
Flaking without itch can suggest a chronic skin condition. If accompanied by inflammation or discomfort, infection should be ruled out.
Rashes (spots, patches, or discoloration)
Genital rashes can be infectious or non-infectious. Common causes include:
- Secondary syphilis: widespread rash that can consist of palms, soles, or genitals
- Scabies or pubic lice: intense itching with small red papules or bite marks
- Trichomoniasis: reddened skin and irritation, especially in women
A rash that doesn’t resolve, spreads, or involves other parts of the body should be evaluated with full STD screening and possibly a skin biopsy.

Blisters (fluid-filled lesions)
Blisters in the genital area are always considered a concerning sign and may point to:
- Genital herpes (HSV-1 or HSV-2): painful blisters that rupture and form crusted sores
- Severe allergic reactions: rare, but may appear after drug exposure
- Autoimmune skin disorders, such as pemphigus vulgaris, though uncommon
Blisters are often painful and may recur in cycles. Early treatment can reduce outbreak severity and transmission risk, particularly with herpes.

What should you do if your genitals itch?
Genital itching is not something to ignore or guess your way through. Whether it’s mild or persistent, any unexplained itch in the genital area deserves a clear explanation—and in many cases, medical attention. Here’s what you need to do.
1. Don’t self-diagnose
Itching is a nonspecific symptom that could indicate an STD, a fungal infection, a skin condition, or an allergic reaction. Treating it blindly with antifungals, antibiotics, or home remedies often delays proper care and can make things worse. Get clarity first, then treat.



2. Eliminate obvious irritants
Stop using anything that could be triggering the reaction: scented soaps, new detergents, lubricants, or tight synthetic underwear. If symptoms ease within 24–48 hours, you may deal with irritation, not infection. But if the itching persists, don’t wait it out.
3. Don’t scratch the area
Scratching may provide temporary relief, but it damages the skin barrier and opens the door to secondary bacterial infections. Use a cold compress instead and avoid friction. If the itch is intense, speak to a provider about antihistamines or topical options.
4. Watch for red flags
Itching rarely happens in isolation. Pay close attention to any of the following:
- Blisters, sores, or bumps
- Redness or swelling
- Unusual discharge
- Burning during urination
- Skin peeling or rash
These symptoms help determine whether you’re dealing with an STD, a yeast infection, or a dermatologic condition—and whether urgent testing is needed.


5. Get tested if you’ve had unprotected sex
If you’ve had unprotected sex, a new partner, or any known exposure, get tested—even if the itching is your only symptom. Many STDs, including chlamydia, gonorrhea, and herpes, start subtly. Early testing is the only way to rule them out confidently and avoid complications.
With Easly, you can order a clinical-grade STD complete test kit online, collect your sample at home, and receive physician-reviewed results with follow-up options.
6. See a healthcare provider
If the itching doesn’t go away within a few days, worsens, or returns after treatment, it’s time to see a doctor. A proper diagnosis may require a physical exam, swab test, urine sample, or blood work. The sooner you get answers, the sooner you get relief.

When to get tested—and what to expect from a test
If you’re dealing with genital itching that doesn’t resolve quickly, or if it’s paired with discharge, skin changes, or recent sexual contact, it’s time to get tested. Delaying STD testing increases the risk of complications and the chance of unknowingly passing an infection to others.
When testing is necessary
You should get tested if any of the following apply:
- You’ve had unprotected sex with a new or multiple partners
- You’re experiencing additional symptoms: discharge, redness, burning, blisters, or rash
- A recent partner has tested positive for an STD
- You’ve been treated for an STD in the past
- You’re unsure whether your symptoms are caused by an STD, yeast infection, or other condition
Testing offers clarity and peace of mind even if symptoms are mild or vague.




What testing involves
STD testing is straightforward, confidential, and tailored to your symptoms and sexual history. Depending on your situation, your provider may recommend:
- Urine test: Used to detect infections like chlamydia or gonorrhea
- Swab test: A sample may be taken from the urethra, vagina, throat, or rectum depending on symptoms and exposure
- Blood test: Required for detecting syphilis, HIV, and herpes antibodies
- Physical exam: In cases of visible symptoms (e.g., sores, warts, or rash), a clinical exam may be enough to identify likely causes before lab confirmation
With Easly, you can collect your sample using medically approved kits, send it to a certified lab, and get physician-reviewed results with follow-up support if needed. Results typically return within a few days. If positive, most STDs are treatable with antibiotics or antivirals. If negative, your provider can help identify other causes, such as fungal infections or dermatological conditions.
Why testing matters
Many STDs are asymptomatic in their early stages, but they still cause internal inflammation and can lead to complications like infertility, pelvic pain, or increased HIV risk. Prompt testing ensures early treatment, protects your partners, and helps prevent long-term consequences.
Conclusion
Genital itching is never just a minor inconvenience; it’s a symptom that deserves your full attention. Whether caused by an STD, a fungal infection, or an external irritant, the only way to get answers is to approach it seriously and clinically.
Several sexually transmitted infections, such as herpes, chlamydia, gonorrhea, trichomoniasis, and syphilis, can present with itch, even before other symptoms appear. But not all cases of itching are infectious. Allergic reactions, hygiene issues, and skin conditions like balanitis or candidiasis can mimic STDs almost exactly.

That’s why self-diagnosis isn’t enough. If your genitals itch, especially with additional symptoms like redness, rash, discharge, or pain, don’t guess. Get tested and talk to a healthcare provider. Rule out what needs ruling out and treat what needs treating.
Sources:
- Centers for Disease Control and Prevention. (n.d.). STD surveillance 2023. U.S. Department of Health & Human Services.
- Centers for Disease Control and Prevention. (n.d.). Trichomoniasis: About.
- National Center for Biotechnology Information. (2019). Sexually transmitted infections
- World Health Organization. (2024, December 11). Over 1 in 5 adults worldwide has a genital herpes infection – WHO.
- World Health Organization. (n.d.). Trichomoniasis.
- CIDRAP. (2024). WHO report shows sexually transmitted infections are climbing. University of Minnesota.