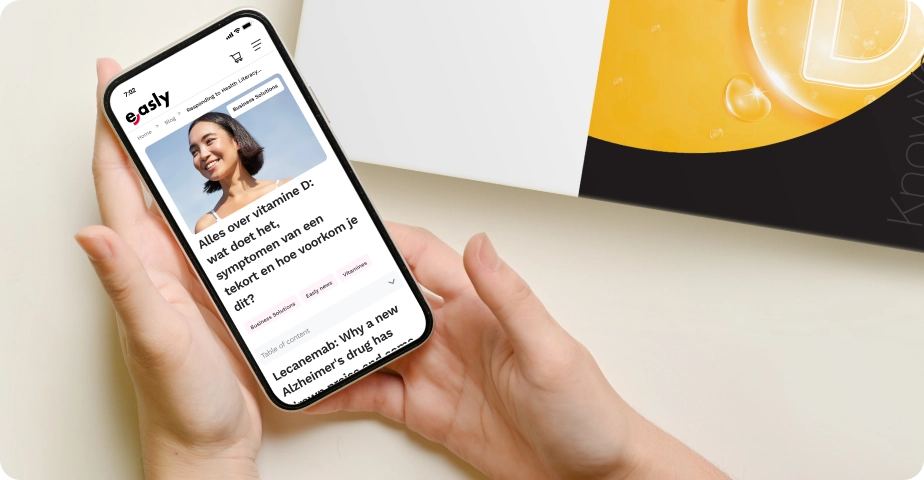
Genital herpes affects over 500 million people worldwide, making it one of the most common sexually transmitted infections (STIs). Despite its prevalence, it remains one of the least understood. The herpes simplex virus (HSV) often hides in plain sight, leading to delayed diagnoses and unnecessary anxiety.

This guide offers a detailed, medically grounded look at genital herpes symptoms, how to get tested, treatment choices, and how to live well with the condition. Whether you’ve just noticed the first signs of genital herpes or are supporting someone who has, you’ll find everything you need to know here.
What is genital herpes, and how is it transmitted?
Genital herpes is a common infection caused by the herpes simplex virus (HSV), which comes in two types: HSV-1 and HSV-2. While both types can infect the mouth and genital area, they differ slightly in how they tend to spread and behave:
- HSV-1 is traditionally associated with cold sores around the mouth, but it is now a growing cause of genital infections. This usually happens through oral sex, as the virus can transfer from the mouth to the genitals.
- HSV-2 is more often associated with genital-to-genital contact and tends to cause recurring outbreaks in the genital area.
The virus spreads primarily through skin-to-skin contact during sexual activity. Unlike many infections that require the exchange of bodily fluids, HSV only needs contact with the skin or mucous membranes. This means it can be transmitted during vaginal, anal, or oral sex, even if no visible sores are present.
One lesser-known fact is that both male and female genital herpes can spread silently. This happens through asymptomatic viral shedding, when the virus is active on the skin without causing noticeable symptoms.

Even with consistent condom use, the risk isn’t eliminated. Condoms cover only part of the genital area, leaving other skin surfaces exposed. That’s why combining safe sex practices with honest conversations about STI status is key to reducing transmission.
The main symptoms of a herpes STD?
Recognizing the symptoms of genital herpes can feel overwhelming, especially if it’s your first experience with them. For many, the signs are subtle at first, or mistaken for other conditions, which can lead to anxiety and uncertainty. But understanding how herpes tends to present itself can help you know what to watch for and when to seek care.

Early warning signs: the prodrome
Before any visible sores develop, you might feel a tingling, itching, or burning sensation in the skin around your genitals, buttocks, or thighs. This phase, called the prodrome, is the virus reactivating in nerve endings. It’s easy to confuse this with irritation from tight clothing or even razor burn, but it’s also when the virus becomes most contagious.
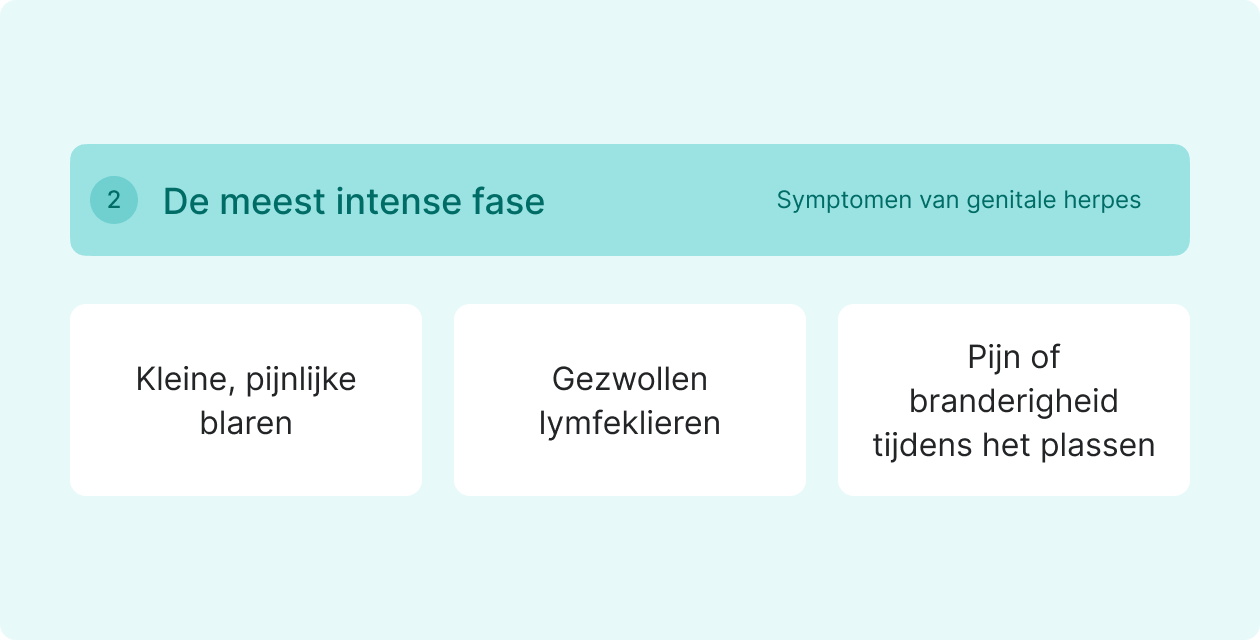
Primary outbreak: the most intense phase
The first outbreak often comes as a shock because symptoms can be more severe. You may notice:
- Small, painful blisters in clusters that rupture and leave open sores.
- Swollen lymph nodes in the groin and flu-like symptoms like fever, headache, etc.
- Pain or burning during urination, especially if sores are near the urethra.
These sores typically heal in 2 to 4 weeks, but tenderness may linger for a few days after.
Why it’s often missed in women
Genital herpes in women, sores can develop internally in the vagina or on the cervix, areas not visible without a medical exam. This can lead to delayed diagnosis or confusion with a yeast infection or UTI. This is different for genital herpes in men whose sores appear on visible areas like the penis, scrotum, or inner thighs, areas that are easier to spot.


When do symptoms usually appear, and how long do they last?
The incubation period for herpes simplex virus, the time from exposure to the appearance of symptoms, ranges from 2 to 10 days, with most people noticing signs around day 4 or 5.
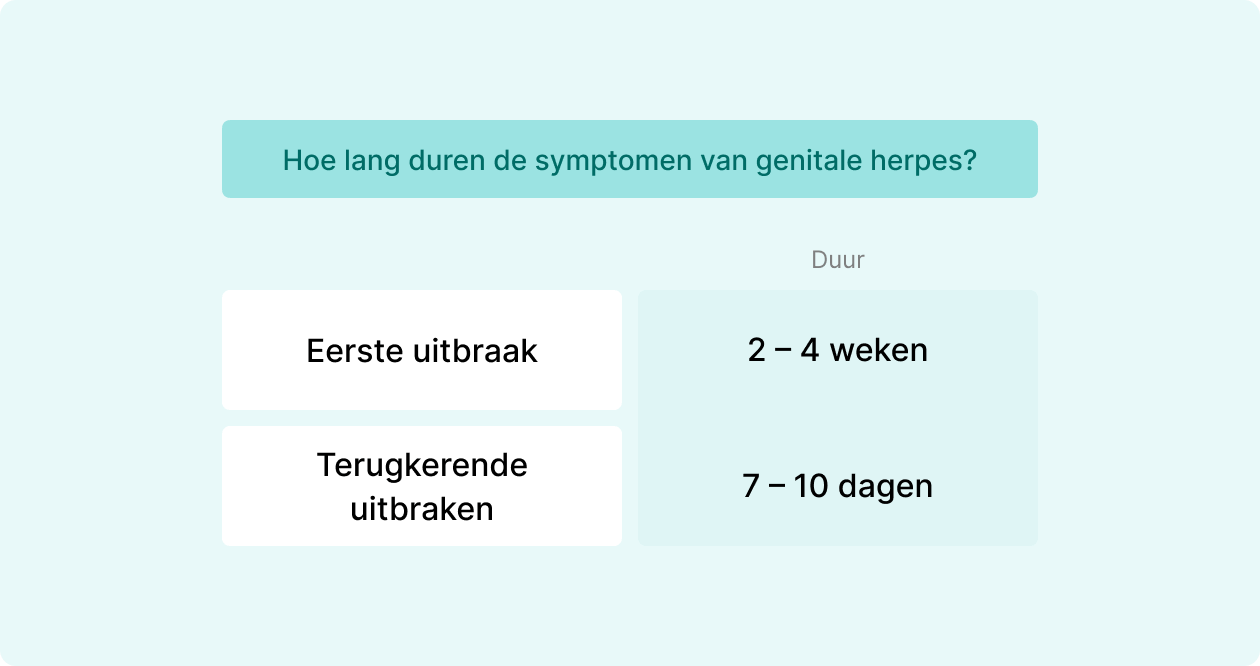
How long do outbreaks last?
- The initial outbreak often lasts 2 to 4 weeks, making it the longest and most intense episode.
- Later recurrent outbreaks are shorter, typically healing within 7 to 10 days and causing fewer lesions.
How often do outbreaks happen?
Recurrence patterns vary widely. Some people may experience several outbreaks during the first year, while others have few or none after their initial episode.
What triggers recurrences?
Common triggers include:
- Physical or emotional stress
- Illness or fever
- Hormonal changes (such as menstruation)
- Friction in the genital area
- Sunlight exposure (more common with HSV-1)



How can someone prevent spreading herpes to others?
Because herpes STIs can spread even in the absence of symptoms, prevention is multi-layered:
- Use condoms consistently, but remember, they don’t cover all skin.
- Take antiviral medication, such as valacyclovir, to reduce viral shedding.
- Avoid sexual activity during active outbreaks.
- Openly communicate with partners about your status.
- Avoid sharing sex toys or disinfect them properly.
Research indicates that daily antiviral therapy can reduce the transmission risk to an uninfected partner by nearly 50%.



Can genital herpes be cured or only managed?
There is currently no cure for genital herpes. Once HSV enters the body, it remains in nerve cells near the spine, lying dormant for long periods and reactivating unpredictably. But living with herpes doesn’t mean constant symptoms or fear of transmission. Over time, most people experience fewer and milder outbreaks as their immune system adapts.
Managing herpes focuses on two key goals:
- Controlling symptoms to minimize discomfort and speed healing.
- Reducing the risk of passing the virus to others.
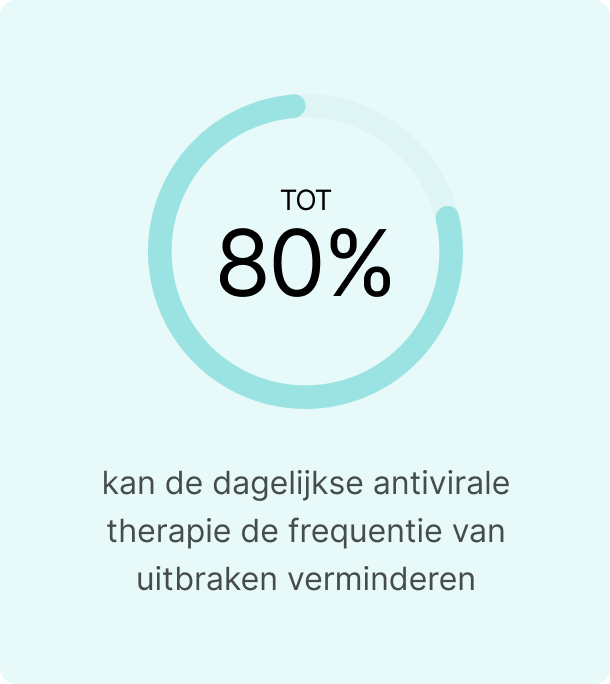

Daily antiviral therapy can reduce outbreak frequency by up to 80% and cut transmission risk nearly in half, allowing people to maintain fulfilling relationships and sexual health.
What treatments are available for genital herpes?
Although a genital herpes cure is not yet available, modern treatments allow most people to keep symptoms under control and live full, confident lives.
Antiviral medications: a powerful tool
Antiviral medications: a powerful tool
Doctors often prescribe antivirals like acyclovir, valacyclovir, or famciclovir to help the body suppress the virus and speed healing. These genital herpes medications are highly effective at reducing pain and preventing new sores from forming.
- Episodic treatment: Start medication at the first sign of tingling or redness to reduce outbreak severity and duration.
- Suppressive therapy: For frequent recurrences, a low daily dose can cut outbreaks by up to 80% and lower transmission risk to partners.




Easing discomfort at home
During an outbreak, supportive care can make a big difference:
- Over-the-counter pain relievers like ibuprofen can reduce pain and fever.
- Warm sitz baths or cool compresses may help soothe irritated skin.
- Loose, cotton underwear helps prevent friction and allows sores to heal.
If you’re worried about passing herpes to a partner, speak with your healthcare provider about preventive treatment options for them as well.

When should someone consider getting tested?
Because genital herpes symptoms are often mild or absent, many people don’t realize they’re infected. Testing is the only way to confirm an infection, and it’s a crucial step for protecting both your health and your partner’s.
Consider getting a genital herpes test if you:
- Notice sores, itching, or burning in the genital or anal area.
- Have a partner diagnosed with herpes genital or who has unexplained sores.
- Are pregnant or planning pregnancy, as herpes can pose risks during delivery.
- Have had unprotected sex and want reassurance about your status.


Even without visible symptoms, the virus can still be present and transmissible. Early testing allows for early genital herpes treatment, reduces the chance of spreading the virus, and provides peace of mind.
How do you get tested for genital herpes
There are two main ways to test for herpes: laboratory testing through a healthcare provider and at-home testing options. Each has its own advantages depending on your situation.
Lab testing: the traditional approach
Healthcare providers typically use one of these tests:
- Swab test – Taken from a visible sore during an active outbreak. This method detects HSV DNA and is most accurate when lesions are fresh.
- Blood test – Measures antibodies against HSV. This is useful if you don’t have active sores but want to know if you’ve been exposed in the past.
A doctor can help decide which test fits your symptoms and sexual health history.


At-home testing: a private, convenient option
For those who prefer more privacy, you can have a genital herpes test online, it’s a discreet discreet alternative to clinic visits. With this method, you receive a kit that let you collect a sample yourself, send it to a certified lab, and access your results securely online.
Providers like Easly offer reliable at-home herpes tests, which can be especially helpful if you live far from sexual health services or feel uncomfortable with in-person appointments. If your results come back positive or unclear, a healthcare provider can guide you on next steps and treatment.
Conclusion
A diagnosis, or even the fear of genital herpes can feel heavy. But it’s important to understand this: herpes is common, and it doesn’t define your health, relationships, or future.
Today’s genital herpes treatments can reduce symptoms, lower transmission risk, and give you back a sense of control. Many people find that, over time, outbreaks become less frequent and less severe. With the right care and support, living confidently is not just possible, it’s expected.
If you’re experiencing symptoms or simply want clarity about your status, getting tested is the first step. Early testing allows for early treatment, protects partners, and removes uncertainty.
If you prefer a private option, herpes STD test kits, such as those from Easly, make it easy to check your status discreetly and take control of your health from home. Whatever path you choose, early testing allows for earlier care, protects partners, and gives you peace of mind.
Your health, and peace of mind are worth it.
Sources
- PubMed. Genital Herpes: Rapid Evidence Review.
- Wikipedia. Genital Herpes.
- Easly. STI at home testing.
- Centers for Disease Control and Prevention. About Genital Herpes.
- Huidarts. Herpes genitalis.
- Healthline. How Long Does It Take for Herpes Symptoms to Appear or Be Detected on a Test?
- Mayo Clinic. Genital Herpes.
- Hims. My Partner Has Herpes: What Are the Chances I’ll Get It?
- Centers for Disease Control and Prevention. STI Treatment Guidelines.
- National Institute for Public Health and the Environment. Genital Herpes.
- Arts en Zorg. Herpes genitalis: wat is het, hoe krijg je het en wat kan je er tegen doen?