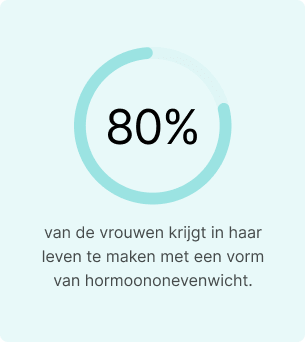
Hormonal balance is foundational to women’s health, yet an estimated 80% of women experience some form of hormone imbalance in their lifetime.
One of the most underdiagnosed, yet far-reaching, is progesterone deficiency. Unlike estrogen, which often receives more attention, progesterone is frequently overlooked in routine hormone assessments. But when levels drop, the impact on health can be significant. Low progesterone can disrupt fertility, destabilize mood, impair sleep, and alter how the body stores and uses energy.
This guide outlines what low progesterone looks like in real-world terms, how it’s tested, and how to restore balance and improve quality of life. Let’s dive in!
What is Progesterone, what does it do, and where is it found?
Progesterone is a steroid hormone made from cholesterol. In women, it’s mainly produced by the ovaries after ovulation, specifically by the corpus luteum, and later by the placenta during pregnancy. Smaller amounts are also released by the adrenal glands.
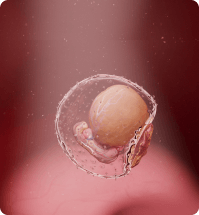
Its primary role in women is to support the second half of the menstrual cycle, known as the luteal phase. After ovulation, progesterone prepares the uterine lining (endometrium) to receive a fertilized egg. If pregnancy occurs, it helps maintain the pregnancy by preventing uterine contractions and supporting the early development of the placenta.
During pregnancy, progesterone levels rise steadily to support the uterus, maintain the placenta, and promote fetal development. It also helps prevent uterine contractions and prepares breast tissue for milk production.


But progesterone does more than support reproduction. It also acts on the brain, interacting with GABA receptors to promote calmness, better sleep, and emotional stability. It helps regulate bone formation by supporting osteoblast activity and contributes to fat metabolism and insulin sensitivity.
In men, progesterone is produced in lower levels by the adrenal glands and the testes. It acts as a precursor to both testosterone and cortisol. It helps balance estrogen, supports sperm development, and plays a protective role in prostate health.

Understanding progesterone levels
Progesterone levels naturally fluctuate throughout the menstrual cycle and pregnancy. In a typical 28-day cycle, they remain low during the follicular phase, rise sharply after ovulation, and drop again before menstruation if pregnancy doesn’t occur.
Here’s how progesterone levels typically look:
- Follicular phase: less than 1 ng/mL
- Luteal phase: 5–20 ng/mL
- Pregnancy: up to 90 ng/mL or more, depending on the trimester
A blood test taken around day 21 of your cycle—roughly seven days after ovulation—can help assess if progesterone rises as expected. In the luteal phase, levels under 10 ng/mL may indicate a deficiency, especially for those experiencing irregular cycles, short luteal phases, or trouble conceiving.


Consistently low progesterone levels during this window can be a sign that the body isn’t producing enough hormones to support implantation or early pregnancy.
Progesterone in men and women: key differences
While progesterone is often associated with female reproductive health, it plays important roles in both sexes. The table below highlights the key differences in function, levels, and effects.
| Aspect | Women | Men |
|---|---|---|
| Production Sources | Ovaries (corpus luteum), placenta, adrenal glands | Testes, adrenal glands |
| Normal Levels | Fluctuates monthly (0.1–20+ ng/mL); higher during pregnancy | Low and steady (typically <1 ng/mL) |
| Main Functions | Regulates the menstrual cycle, supports pregnancy, balances estrogen | Precursor to testosterone and cortisol, regulates estrogen levels |
| Deficiency Symptoms | Irregular periods, PMS, fertility issues, anxiety, poor sleep | Fatigue, low libido, mood changes, prostate enlargement risk |
Note: Too low progesterone in both men and women can impact more than reproductive health. It affects mood regulation, metabolism, and even long-term hormonal balance. Addressing a deficiency early can help reduce broader health risks.
Can I get pregnant with low progesterone levels?
Yes, but it’s more difficult, and sustaining a pregnancy can be challenging.

Progesterone prepares the uterine lining for implantation and helps sustain it afterward. If levels are too low during the luteal phase, the endometrium may not be receptive enough for a fertilized egg to implant successfully. Even if implantation occurs, low progesterone has been linked to an increased risk of early miscarriage, particularly in the first trimester.
Can you ovulate with low progesterone?
It’s possible to ovulate and still have low progesterone afterward. This is known as a luteal phase defect, where the body releases an egg but doesn’t produce enough progesterone to support implantation. Ovulation tests and temperature tracking can confirm when ovulation happens, but they don’t show whether hormone levels are high enough. Only a blood test about a week after ovulation can confirm that. If your cycles are short, you spot before your period, or you’re having trouble getting pregnant, low progesterone after ovulation could be the reason.



What does progesterone do to your weight?
Progesterone helps regulate fluid balance, appetite, and metabolism. When levels drop—especially in relation to estrogen—it can lead to water retention, increased cravings, and fat accumulation around the abdomen.
This imbalance is particularly common during perimenopause and menopause, when progesterone declines more rapidly than estrogen. As a result, many individuals experience slower metabolism, increased abdominal fat, and greater difficulty maintaining a stable weight.


How do you increase your progesterone?
If you are experiencing a decrease in progesterone levels, there are several ways to support hormone production naturally, especially if you’re still ovulating regularly. But in more severe cases, medical treatment may be necessary.
Here’s what can help:
- Manage stress: Chronic stress raises cortisol, which shares the same hormonal precursor (pregnenolone) as progesterone—diverting resources away from its production.
- Prioritize key nutrients: Vitamin B6, magnesium, and zinc are essential for hormone synthesis. Foods like leafy greens, legumes, and seeds can help support optimal levels.
- Exercise in moderation: Regular movement supports hormone balance, but overtraining can suppress ovulation and reduce progesterone output.
- Herbal support: Chasteberry (Vitex agnus-castus) has been shown to improve luteal phase progesterone in some women, though results vary.
- Medical therapy: In moderate to severe cases—especially with confirmed luteal phase deficiency, infertility, or perimenopausal symptoms—bioidentical progesterone may be prescribed. This is the most effective way to restore hormone levels when natural production is insufficient.




Note: While lifestyle changes and supplements can support hormone balance, they cannot replace medically prescribed progesterone when clinically indicated. Speak with your healthcare provider to determine the best course of action based on your symptoms and test results.

Progesterone deficiency testing
The first step in diagnosing progesterone deficiency is accurate testing. This is especially important if you are experiencing fertility challenges, irregular cycles, or symptoms of hormonal imbalance.
One of the methods used is a blood test performed around day 21 of a 28-day cycle, corresponding to about 7 days after ovulation. This timing captures peak progesterone during the luteal phase. For added convenience, clinical-grade at-home testing is also available. The Easly women’s hormone test uses a saliva or blood spot sample to measure key hormone levels, including progesterone and estrogen.
It offers medically supervised results with lab-grade accuracy, making it a practical first step toward diagnosis, especially when traditional lab access is limited.
In summary
Progesterone plays a central role in fertility, menstrual regulation, mood stability, and metabolic function for both women and men. When levels fall too low, the effects can manifest as irregular cycles, difficulty conceiving, anxiety, poor sleep, or weight changes.

The good news is that progesterone deficiency can be identified and managed with the right testing and evidence-based treatment. Early diagnosis and treatment can improve reproductive outcomes, emotional health, and long-term hormonal stability.
Concerned about your symptoms? The Easly’s at-home hormone test offers a simple, clinical-grade way to check your progesterone levels from home.
Sources:
- American College of Obstetricians and Gynecologists (ACOG). – Progesterone and Its Role in Women’s Health.
- Endocrine Society. – The Role of Progesterone in Hormonal Balance.
- Mayo Clinic. – Progesterone Deficiency Symptoms and Treatment.
- National Institute of Child Health and Human Development (NICHD). – Progesterone: A Hormone that Supports Pregnancy.
- The Hormone Health Network. – How Progesterone Affects Women’s Health.
- Journal of Clinical Endocrinology and Metabolism. – Progesterone and its Role in Reproductive Health.
- Easly Health. – At-Home Hormone Testing for Progesterone.