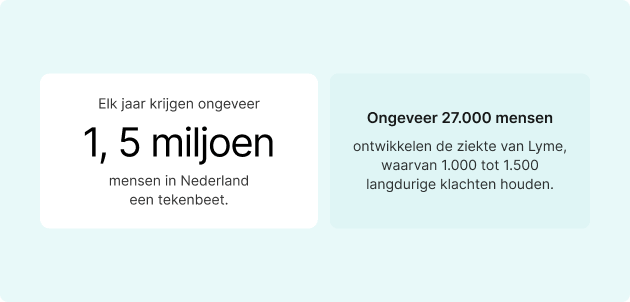
Tick bites often go unnoticed – but that doesn’t make them harmless. Although most only cause mild skin reactions, some ticks carry pathogens that can cause serious conditions, such as Lyme disease. Every year, approximately 1.5 million people in the Netherlands are bitten by ticks. Approximately 27,000 people develop Lyme disease, of whom 1,000 to 1,500 experience long-term symptoms.
As ticks spread to new areas, it is more important than ever to recognise the symptoms of a tick bite – and to know when to seek medical attention. In this article, you will learn how to recognise a tick bite on the skin, what symptoms may indicate an infection, and what signs indicate that you should consult a doctor. Let’s get started!

What is a tick?
Ticks are small, spider-like parasites that feed on the blood of animals and humans. They belong to the arthropod family and have eight legs. Before feeding, they vary in size from a poppy seed to about a sesame seed. Once they attach themselves and fill with blood, they can swell considerably, making them easier to spot.
Ticks are not insects – they are classified as ectoparasites and are commonly found in wooded, grassy or damp outdoor environments. They do not jump or fly, but wait on plants for a host to pass by, at which point they attach themselves.


Are ticks dangerous?
Yes, ticks can pose a serious health risk. Although not every tick bite leads to illness, some ticks carry pathogens that can be transmitted to humans through a bite. Lyme disease is the most well-known, but different species of ticks can also spread diseases such as tick-borne encephalitis (TBE), babesiosis, ehrlichiosis and Rocky Mountain spotted fever.
What does a tick bite look like? Can you feel a tick bite?
Understanding what happens when you are bitten by a tick – from skin reaction to risk of infection – helps you take the right steps if a bite goes unnoticed, symptoms appear or medical care is needed.
Unlike mosquito or flea bites, tick bites are usually painless. This is because ticks secrete a mild anaesthetic in their saliva, which allows them to attach themselves unnoticed and feed for hours or even days.
In the early stages, a tick bite often appears as a small, red bump, similar to a mosquito bite. If the tick is still attached, you can see its body protruding from the skin. After removal, the area may remain red or slightly swollen for several days.


In some cases, however, a characteristic rash develops. The best known is the ‘bull’s-eye’ rash (erythema migrans), a classic sign of Lyme disease. This rash usually appears 3 to 30 days after the bite and gradually spreads with a central clearing.
Other possible symptoms around the bite site include:
- Redness or swelling
- A crust or flaking (especially if scratched)
- Warmth or tenderness (less common, unless infected)
A tick bite on human skin requires careful monitoring. Inspect your skin – and that of your child or pet – after spending time in areas where ticks are prevalent, so that you can catch any bites early.

What are the most common diseases caused by tick bites?
Not every tick bite leads to illness, but when a tick carries pathogens, it can transmit serious diseases. The table below provides an overview of the most common tick-borne diseases, their causes, symptoms and geographical distribution:
| Illness | Pathogen | Main symptoms | Type of sign | Regions |
|---|---|---|---|---|
| Lyme disease | Borrelia burgdorferi | Target shooting results, fatigue, fever, joint pain | Black shoulder tick (deer tick) | United States, Europe, parts of Asia |
| Tick-borne encephalitis (TBE) | TBE virus | Fever, headache, neurological symptoms (e.g. meningitis) | Ixodes tick | Central and Eastern Europe, Scandinavia, Russia |
| Babesiosis | Babesia parasites | Fatigue, chills, anaemia, muscle pain | Black shoulder tick | Northeast and Midwest US, Europe |
| Ehrlichiosis | Ehrlichia bacteria | Fever, chills, headache, muscle pain | Lone Star tick | US (South Central, Southeast) |
| Anaplasmosis | Anaplasma bacteria | Fever, chills, muscle pain, confusion | Black shoulder tick | Northeast and North-Central United States |
| Rocky Mountain Spotted Fever (RMSF) | Rickettsia rickettsii | High fever, blotchy rash, nausea | American dog tick, Rocky Mountain wood tick | US (Southeast, South Central) |
| Alpha-Gal Syndrome | Allergy to red meat caused by tick saliva | Symptoms, stomach complaints, anaphylaxis after eating red meat | Lone Star tick | Southeast and Central United States |
What are the symptoms of a tick bite infection in humans?
Below are the most common symptoms of a tick bite to look out for.
Early systemic symptoms
- Fever and chills
- Fatigue or general weakness
- Headache
- Muscle or joint pain
- Swollen lymph nodes
These flu-like symptoms can be confused with a viral infection, so it is important to mention any recent tick exposure to your healthcare provider.



Serious symptoms
If the infection spreads or remains untreated, the symptoms may worsen:
- Facial paralysis (facial paralysis or Bell’s palsy)
- Stiff neck or severe headache
- Cognitive changes such as confusion or concentration problems
- Tingling or numbness in the limbs
- Heart palpitations or chest discomfort (associated with Lyme carditis)


If any of these symptoms appear, especially after outdoor activities or exposure to ticks, seek medical attention immediately.
How do you remove a tick that is already under the skin?
If you find a tick on your skin, it is important to remove it as quickly as possible. The longer a tick remains attached, the greater the risk of disease transmission, especially after the first 24 hours.

Step-by-step sign removal
Follow these steps, recommended by health authorities such as the CDC:
- Use fine-tipped tweezers: Grasp the tick as close to the skin as possible.
- Pull slowly and steadily straight up: Avoid twisting or pulling, as this may cause parts of the tick to break off and remain in the skin.
- Clean the bite area and your hands: Use soap and water, alcohol or an iodine solution.
- Dispose of the tick properly: Flush it down the toilet, put it in alcohol, or store it in a plastic bag for possible identification later.
- Do not use home remedies: Avoid Vaseline, nail polish, matches or essential oils – these do not help and may irritate the skin or increase the risk of disease.



Read more in the tick removal guide from the CDC.
Please note: Incorrect removal, such as squeezing the tick’s body, twisting it or applying oils, can increase the risk of infection or disease transmission. Always follow the instructions carefully to avoid complications.
What if the head breaks off?
If parts of the tick remain behind:
- Try to remove them with clean tweezers.
- If this does not work, leave the area alone — your body may reject it on its own.
- Watch for signs of infection such as redness, pus or increasing swelling.
How can you recognise an infected tick bite?
An infected tick bite is not the same as a tick-borne disease, but both require attention. Infection can be localised, affecting only the skin, or systemic, affecting the entire body through pathogens transmitted via the tick’s saliva.

Signs of a localised skin infection
A typical tick bite may cause mild irritation. However, if bacteria enter the skin, the following signs of a local infection may appear 1–3 days after removal:
- Increasing redness or swelling
- Increased pain or warmth
- Yellow pus or fluid accumulation
- Smooth, tense skin around the bite
- A bite that worsens after initial improvement
These symptoms may indicate cellulitis or another bacterial skin infection and require medical attention.
Systemische infectie: voorbij de beet
Tick-borne diseases such as Lyme disease, ehrlichiosis or anaplasmosis may not cause any obvious symptoms at the site of the bite. Instead, they affect the entire body.
Please note the following:
- Persistent or recurring fever
- Fatigue, chills or muscle pain
- Headache or stiff neck
- Swollen lymph nodes or joint pain
- Ring-shaped rash (erythema migrans)
- Numbness, confusion or drooping face




These symptoms often appear within 3 to 30 days after a tick bite. Consult a healthcare professional promptly for early treatment to reduce the risk of complications.
If symptoms such as fatigue or headaches persist after treatment, a home test can help to detect any remaining disturbances and support recovery.
When to see a doctor
Many tick bites heal on their own, but some can lead to serious complications. Knowing when to take a tick bite seriously will help you act early and prevent long-term effects. Seek medical attention immediately if you:
- You have a spreading rash, especially if it resembles a bull’s-eye
- You develop a fever, fatigue or muscle pain after spending time in grassy or wooded areas
- The bite site becomes increasingly red, swollen or painful
- You experience neurological changes, such as facial paralysis or confusion
- You are unsure how long the tick was attached
- You did not remove the tick completely
If symptoms such as fatigue or a slow recovery persist after treatment, Personalised Blood Test can help identify any remaining problems and support further care.

How to prevent tick bites
Ticks thrive in grassy, wooded and bushy areas – and they don’t need much time to attach themselves. But with the right prevention strategy, tick bites can be largely avoided. These scientifically proven measures can protect you, your family and your pets from ticks.
1. Use proven repellents
Apply an EPA-approved insect repellent spray to exposed skin before going outside. The most effective ingredients are:
- DEET (20–30%)
- Picaridin
- IR3535
- Lemon eucalyptus oil (not suitable for children under 3 years of age)
Always apply repellents according to the instructions on the packaging. For long-lasting protection, wear clothing treated with permethrin, an insecticide that repels ticks and kills them on contact.


2. Dress to limit exposure
Ticks crawl up from the ground, so your clothing is your first line of defence:
- Wear long sleeves and long trousers
- Tuck your trousers into your socks or boots
- Choose light-coloured clothing — ticks are easier to see
- When walking in nature, stay in the middle of the paths and avoid contact with tall grass or bushes
3. Perform thorough tick checks
Check yourself thoroughly after outdoor activities, especially in areas where ticks are common, for ticks on:
- The scalp and hairline
- Behind the ears
- Under the arms
- Around the waist and groin
- Behind the knees
- Around the ankles and socks
Parents should keep a close eye on their children, and pet owners should inspect their animals’ fur, ears and paws.



4. Shower within two hours
Showering shortly after being outside helps wash away ticks before they bite. It is also a good time to thoroughly check your skin under good light.
5. Keep ticks out of your home
Reduce the habitat of ticks around your home by:
- Mow the grass regularly
- Remove leaves and piles of branches
- Move wood piles and birdhouses away from terraces and play areas
- Create a buffer of gravel or mulch between the lawn and wooded areas
6. Protect pets all year round
Ticks don’t just affect humans. Use preventive measures recommended by your vet for dogs and cats, such as:
- Oral medications
- Tick bands
- Topical treatments


Pets can bring ticks indoors, increasing the risk for the entire household.
What does progesterone do to your weight?
Tick bites are often overlooked, but can lead to serious infections. Although not all ticks transmit diseases, some can cause conditions such as Lyme disease or tick-borne encephalitis. Early recognition and quick action are therefore essential.
After a bite, watch out for symptoms such as fever, rash or fatigue. If these symptoms appear, consult a doctor immediately. Early treatment can prevent complications and reduce the risk of long-term effects.

fatigue or concentration problems (brain fog). In such cases, home tests for immune, hormone or nutrient markers can provide valuable insights for recovery and further care.
Stay alert, act quickly and give your body the right support to recover. Awareness and proactive care are your best protection against tick bites.
Sources:
- Centers for Disease Control and Prevention. (2025, March 13). Lyme Disease Surveillance and Data.
- Centers for Disease Control and Prevention. (2024, May 14). Tick-borne Encephalitis Virus.
- Centers for Disease Control and Prevention. (n.d.). Babesiosis.
- Centers for Disease Control and Prevention. (2024, May 15). About Rocky Mountain Spotted Fever.
- Healthline. (n.d.). Lyme Disease: Symptoms, Signs, Treatment, and More.
- Centers for Disease Control and Prevention. (2024, May 15). Signs and Symptoms of Untreated Lyme Disease.
- Centers for Disease Control and Prevention. (n.d.). Tick Removal.
- New York State Department of Health. (n.d.). Lyme Disease.
- Prince William County, Virginia. (2021, April). Repellent Combined.
- RIVM – Ziekte van Lyme
- Tekenradar